By Thomas Myers
Originally published in Massage & Bodywork magazine, October/November 2006.
The word posture, which comes from the Latin placement, is used to describe how we stand in space, and it is a good enough word for common use: “His sunken posture conveys defeat.” Or for metaphoric use: “Our posture toward Iran is evolving,” meaning attitude. But for those of us in the massage and bodywork trade, especially those who wish to, or claim to, change posture for the better, the term will not stand up to close examination.

What we commonly call posture is instead a pattern of movement. Moshe Feldenkrais coined the word acture to describe posture in action (see Figure 2, page 44). First, standing or sitting still is, in fact, an action, and we are never placed in stillness; we are always moving, shifting, balancing, adapting—even in the stillness of meditation. It’s in our nature; the utter stillness of an actual posture will always be denied us while we still breathe. Your first posture will be the one you die in. (And even then the inner movement continues—read Mary Roach’s crazy/wonderful Stiff [Norton, 2003]).
Secondly, we never do it exactly the same way twice, as we adapt to a particular seat, or shoes, or circumstance. Thirdly, the range of our posture varies with the time of day (we’re all shorter in the afternoon, for instance) and our inner attitude (fear, eagerness, fatigue).1
So we have a range that we move through—a postural set if you will. That range is familiar to those who know us. See a friend walking a couple of blocks down the street, or see someone doing anything—shoveling, on a swing, pulling on boots—and your brain’s movement sense can create recognition and identify that person without seeing her face or hearing her voice.
(The brain’s sense of seeing movement was the first form of vision to evolve. The visual senses of line, form, and color we take for granted came later. Our brains are very adept at differentiating various movements, honed over millennia of hunting and being hunted. This information even takes a different pathway, down through the reptilian brain on its way to the occipital lobe. You can often sense movement better by watching with your peripheral vision: look at something else and assess the client’s movement from the corner of your eye.)
So, I use acture—not a real word, but it should be —because I think Moshe hit this nail on the head: posture is always in action, and the characteristic relationships among body parts are commonly maintained in all kinds of different movements and actions. Reaching into the neurology, physiology, and the fascial “stuckness” of these patterns is the job of those of us who labor in the vineyard of changing posture.2
That said, let us look at a few of the greatest hits (or call it Tom’s playlist) in the realm of actural issues with which we commonly deal. Since this is a column, we will have to address them shortly, but each is written about more fully in books and other articles, which are referenced here.
Actural Issues:
Head Retraction
The first, most common, and perhaps the most damaging, actural pattern is head retraction, commonly associated with Head Forward Posture, or HFP (see Figure 3). Chronic contraction of the suboccipital muscles, which pulls the back of the head toward the upper neck and back, creates many postural problems, all of which relate to HFP. Though HFP is often associated with fear (both the startle response and the Landau [extension, flight] reflex), such a pattern can also be caused by poor vision, the desire to please, airway obstruction, back pressure issues, or malocclusion of the jaw, to name the more common causes.

Correcting this pattern of chronic and reflexive upper cervical hyperextension is a mainstay of the Alexander Technique and the focus of sustained interest in both osteopathic and chiropractic approaches, as well as the Rolf-evolved methods. Without length in this area, the eyes lose their coordination to the spine, and our natural spring and grace are lost. Lengthening these small, highly innervated muscles, as well as activating their partner the anterior scalene, is essential business for most of our clients in order to get their head on straight.3
The Two Diaphragms
Secondly, we can look for reciprocity between the two abdominal diaphragms—the respiratory diaphragm and pelvic diaphragm (pelvic floor). In a relaxed and balanced acture, the two diaphragms face each other, like the top and bottom of a beach ball, or the two hands in someone practicing tai chi (see Figure 4). Commonly, in a swayback (lordotic) acture, the two diaphragms will both aim forward. In the less common flat back (flexed) pattern, the two diaphragms can aim backward, again missing each other. Sometimes the rib cage can be shifted forward or (more commonly for us Westerners) backward relative to the pelvis, and these two diaphragms again lose their reciprocity.

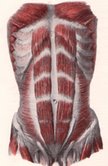
This loss has detrimental effects on breathing, of course, but also multiple and nefarious effects on digestion and organ function in the pelvis, causing congestion around the kidneys and sexual organs which then creates deleterious long-term preconditions for disease. The pelvis’s relation to the legs and the rib cage’s relation to the shoulders figure into this equation, but the primary actor in this arena is what I call the four pillars (a bad name as they are heavy fascial tensile strings not compressive bony pillars, but you know how nicknames stick). The pillars are the two lateral raph»es in back (see Figure 5A), just lateral to the erectors, where the abdominal fasciae and the back fasciae meet, and the longer strings of fascia in the front in the abdominal fasciae, just outside the edges of the rectus abdominis (see Figure 5B). Getting the balance of these four pillars right goes a long way to ensure a better balance between the respiratory diaphragm and the smaller pelvic one.

Getting these two diaphragms balanced one over the other is also a natural result of good Pilates work, which strives to strengthen and balance what we just called the four pillars via very specific abdominal exercises. But it’s not just a matter of looks: when the organs are contained in a balanced way—a balance of the back muscles, the psoas complex, and the abdominals—breathing is supported, the organs and glands in the abdomino-pelvic cavity are properly pressured and tend to work better, and the lumbar spine is freed to support the heavy structures of the shoulders and head above.4
Pelvic Balance
The third major issue—we are more or less moving down the body, since each of these issues is important—is getting the pelvic balance right relative to the feet and legs.
(“What a minute! If your subject is posture and you’re moving down the body, how can you leave out shoulders? Lots of people these days have terrible shoulder posture.” Yes, that’s true—so much driving and computer jockeying leaves many shoulders weak and out of place, and thus prone to injury and dysfunction. But if you solve the first two issues we’ve brought up—lengthening the neck and balancing the abdominal balloon—75 percent of those shoulder problems will just melt away without a lot of manual work. It works in reverse as well—fail to address these core issues and all your lovely and skilled work on the shoulders themselves will fail to sort out the problems, because the shoulders hang off the neck and rest on the rib cage, so without these central supports, the peripheral appendage can’t work properly.)
In a human, the pelvis serves as the steadying foundation for the spine and simultaneously as an upper girder for the movement of walking. This unique set of design constraints makes the human pelvis a puzzling marvel of biological engineering and the object of study for osteopaths, chiropractors, orthopedists, and the wide variety of movement teachers. Each seems to have his own key or secret to proper pelvic function, but there is as yet no consensus on proper pelvic balance in acture.
Pelvic tilt refers to the angle between the pelvis and the femur. Let us ignore right/left tilts for the moment, and all its concomitant complex issues of leg length, sacral shear, and the effects on the spine, in order to concentrate for a moment on anterior/posterior tilts—the rocking of the pelvis forward and back on the heads of the femurs.
Pelvis means bowl, and an anterior tilt means hip flexion—the pubic bone going down, so that the milk would spill from the front of the bowl. This pattern is, of course, associated with a swayback or lordotic pattern of the lumbars. In a posterior tilt, the milk would spill out the back, as the hips are extended, the lumbars are flat, and the posterior iliac crest is lower than expected relative to the pubic bone.
But how far, exactly? Various posture experts, notably Florence Peterson Kendall, have postulated that the ideal neutral for the pelvic tilt is to have the anterior superior iliac spine and the pubic bone in the same vertical (frontal) plane.5 Ida Rolf asserted that the pelvis is horizontal when the bottom of the tailbone was level with the top of the pubic bone (see Figure 6).6

Personally, I find these measurements too geometric, with insufficient recognition of the variation among humans and what might work for different people.
So I offer the following test as one I use that allows for individual differences and does not try to fit everyone into the same box. It offers up some surprising results sometimes—people you think look anterior tilted turn out to be posterior and vice versa.
Test
Cup your hand and rest it ever so gently on top of your client’s head as she stands quietly, almost resting in her hair, just barely touching the head, so that you can be very sensitive to changes in head position. From her “normal” have her tilt the pelvis slowly anteriorly, then back to normal, then posteriorly and back to normal.
As much as possible, confine the client’s movement to the pelvis. If the client is shifting her knees, dropping the rib cage back, or retracting the head, the test won’t work as well—for this reason, this test works better the freer and more supple the person is. If the client is truly rocking just the pelvis back and forth slowly, you should feel the head rising into your hands and then falling away.
Where is the top of the arc? The point where the pelvis is in the best position is where the head is highest into your hand. That’s why you have to be very sensitive and poise your hand carefully just on the head—so that you can feel changes in height measured in millimeters. If the client’s head is at its highest at normal, then the pelvis is positioned best for them. If the height increases as she moves into an anterior tilt—remember, isolating the pelvic movement, leaving the rest of the body at rest—then normal is too posteriorly tilted for her. If the client lengthens into your hand as she tucks her tail under, then normal is too anteriorly tilted. Confirm your findings by having the client do it a few times—you are looking for the more consistent result.
This functional (rather than geometric) measure of pelvic position works well for me in practice, and can be quite surprising sometimes when you compare it to the normal visual cues we use. The test answers the question: in what pelvic position is the spine freed to be at its longest? The spine living its full length is the higher value, not having the pelvic angle conforming to someone’s idea of good posture.7

In general, spinal length is a strong value in good acture. Even a minor collapse or shortening in the spine, and/or in the organic core that hangs from its front, can have deleterious long-term effects on health and well-being. In a healthy body, the organs are free to move over each other like well-oiled balloons with every breath, and the spine is sprung into the air like one of Kenneth Snelson’s tensegrity structures.8 Proper (and personally adjusted) pelvic position is essential to both these deeper goals.9
Prehensile Feet
Finally, is the issue of feet. Shoulders may have ubiquitous bad positioning, but what happens to feet in our society is positively iniquitous. Shut up in leather coffins all day, or bound tightly in mis-sized running shoes while we pound on them, our society’s feet, while not as deformed as Chinese women’s of former times, verge on the same set of problems. I am not advocating an atavistic devolution when I say we need feet more like monkeys. We need prehensile feet. Partially I mean just what I say—toes should be more mobile and able. Ruthie Alon (a mega-movement teacher from the Feldenkrais tradition) had us tearing up newspapers into small strips using only our toes. What agile feet I had after that! Toes are so jammed together and superfluous in our culture. Bring back the toes! The yoga teacher Kali Ray can interlace her toes (all five)—without the use of her fingers—in fact, while in a handstand (see Figure 8, page 52)! Just sits there and does it while talking about yoga philosophy. No, I can.10

But such prehensility can also extend into the arch. Some feet just go flat, while others have the arch supported by the mechanics of the shoe or extra arch supports. Neither are vital, active arches. To create great arches that offer sufficient support for the superstructure above, there needs to be a slight but active “feeling your ground” in the tarsum of the foot.
I definitely do not mean a white-knuckled grip on the ground with the toes—that’s not healthy. In a proper posture, the toes simply rest on the ground—awake, but not tense. But in the foot itself, a slight feeling of gathering—as if there was another yoga banda in the feet—in the middle of the arch lends an alertness and springiness to the arches, and harkens back to when your feet were your “ear to the ground” as we walked over uneven and variable surfaces, not cocooned in synthetic materials cruising over man-smoothed surfaces. Try it with your hand—the slight feeling of gripping in the palm as if testing or hefting an orange—and then try to get the same feeling with your feet. Keeping that feeling in your feet as you go about your daily business is a good meditation for those with “dead” feet.
Spatial Medicine
From living feet to a lifted cranium, we have hit the high points of posture as I perceive them, thirty years (just getting started) into my practice. Length and alignment are the overarching values that allow posture/acture to become an active contribution to your health, rather than a strain on it.
The more human use of the human body is the great challenge of our time—spatial medicine, I call it. How do we get body mechanics right for a headlong populace in an urban environment? Bad posture/acture contributes a large share to human misery, and it is so unnecessary. How can we most easily transform it? We are all working on this one person at a time, and we all know how slowly that works.
In our next column (and our last column in this series, at least while I write my next book), we will look at what I have found to be the most effective and natural way to build good posture—from the beginning.
(Author’s note: With the cooperation of Massage & Bodywork, I am publishing a collection of the Anatomist’s Corner articles, including those referenced herein. To find this collection, visit www.anatomytrains.net.)
Thomas Myers has practiced integrative bodywork for nearly thirty years. He teaches workshops internationally on anatomy, movement, and soft-tissue work. His book, Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists, was published by Elsevier in 2001. He lives, writes, and sails on the coast of Maine.
Notes
1. You can read more about the art of changing posture in the Anatomist’s Corner article on The Anatomy Trains recipe (Massage & Bodywork, June/July 2004, page 80) or—as a self-help project—in Mary Bond’s new book Heal Your Posture (Inner Traditions, 2006).
2. You can read more about acture in Moshe Feldenkrais’s The Potent Self, page 108ff. (Frog Books, distributed by North Atlantic, 1985.)
3. You can read about the suboccipitals in detail in Massage & Bodywork, October/November 2002, page 98.
4. You can read more about the reciprocity of the diaphragms in a couple of my Anatomist’s Corner articles in Massage & Bodywork: August/September 2000 (“Cups and Domes”) and February/March 2003 (“The Plywood Principle”).
5. Muscles, Testing and Function, 3rd edition, Florence Peterson Kendall and Elizabeth Kendall McCreary, Williams & Wilkins Baltimore, 1983, page 25.
6. Ida Rolf, Rolfing (Rochester, VT: Inner Traditions, 1977), 102.
7. Some issues in pelvic repositioning are dealt with in Anatomist’s Corner columns in the following back issues of Massage & Bodywork: February/March 2001, April/May 2001, June/July 2001, August/September 2001 (all on the psoas and its friends), December/January 2003 (the femoral triangle), and June/July 2003 and August/September 2003 (on the deep lateral rotators).
8. Jean-Pierre Barral and Pierre Mercier, Visceral Manipulation (Seattle: Eastland Press, 1988). Snelson’s versatile artwork is available online at www.keneethsnelson.net.
9. To learn more about the body as a tensegrity structure, read Body3, available from www.anatomytrains.net, or go to www.intensiondesigns.com, www.childrenshospital.org/research/ingber, or www.biotensegrity.com for great pictures and models.
10. Ruthy Alon, Mindful Spontaneity (Berkeley, CA: North Atlantic, 1996); for information on Kali Ray, visit www.triyoga.com.




