By Ben E. Benjamin
Originally published in Massage & Bodywork magazine, December/January 2006.
Pain in the back — primarily the low back — is the source of great suffering and disability for a large number of Americans. Each year, it accounts for more than 70 million visits to doctors. For such a prevalent complaint, low-back pain remains remarkably difficult to explain and treat. Many people claim to understand the root causes, but in my view the real reasons remain a mystery. A number of experts say low-back pain is strictly a mechanical phenomenon, i.e., just fatigue and strain of muscles, tendons, or ligaments. Some blame the problem on imbalances caused by the psoas muscle, while others point to intervertebral discs as the primary culprits. Another theory attributes most low-back pain to emotional stress. Each of these explanations is probably correct some of the time, but none of them tells us why these strains and injuries occur or why they occur with such frequency.
Theories about treating low-back pain are just as varied as theories about its causes. There are claims of success for many different interventions, from massage to surgery, but even after treatment, back pain tends to recur periodically for years. While there is no doubt that some forms of treatment are more effective than others, we often don’t know why and often can’t predict what will work best for each person. For example, it is clear that some people are helped by daily exercise regimes, but others are not. In many cases, injections seem to work wonders, yet in similar cases they may not work at all. And although massage helps many clients feel better, it makes some clients worse.
In this and the following articles, I’ll provide some insight into this puzzling phenomenon and what role massage therapists can play in helping those suffering from low-back pain. First, let’s take a look at the structure of the low back.
Low-Back Structure
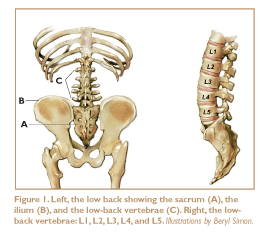
Most people aren’t clear about where their low back begins and ends. In an average-sized adult, the low back is about six inches long. It is bordered by the bottom of the rib cage, the top of the hip bones, and the superior portion of the sacrum. Functionally speaking, the low back consists of two segments that work together: the five lumbar vertebrae (L1, L2, L3, L4, and L5) and the sacrum (Figure 1).
We will focus here on the areas around the vertebrae and address problems of the sacrum in a future article.
Natural Alignment and Structural Abnormalities
In a normal, healthy spine, the five lumbar vertebrae form a forward (lordotic) curve, so that when you lie supine with your legs straight you can easily slide your hand under your low back. A low back without this natural, shock-absorbing curve is out of balance and has less stability. A reverse curve, in which the vertebrae are straight or curved posteriorly, can make a person more prone to back pain.
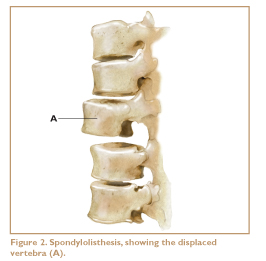
In some cases, instability is caused by loose ligaments. The function of ligaments is to hold our bones together in order to keep our joints stable. Ligaments, unlike muscles, need to be tight to do their job effectively. When ligaments are loose (i.e., longer than they should be), our bones and joints become unstable. Some people are born with ligaments that are loose. Ligaments can also become stretched as a result of injury. The spinal ligaments are supposed to hold the vertebrae together tightly. Abnormal lengthening of these ligaments can be a contributing factor in back pain. One structural problem associated with such lengthening is called spondylolisthesis — (pronounced spon-di-low-lis-thee-sis). This is a congenital condition in which one or more of the vertebrae are substantially misaligned (Figure 2).

A vertebra may be one-quarter to one-half inch out of alignment, anteriorly or posteriorly, instead of sitting squarely on the vertebra below. While this deviation may sound small, it can create a great deal of difficulty. Individuals with spondylolisthesis are more vulnerable to injuries to the spinal ligaments and discs. This condition occurs more frequently in the low-back region than in other parts of the spine.
Scoliosis, an exaggerated sideways S curve of the spine (Figure 3), is sometimes cited as a cause of back pain, but this is seldom true. Extreme scoliosis causes severe pain problems and often requires surgery, but the common variety rarely causes problems in the low back. Low-back pain is no more common in individuals with slight scoliosis than it is in those without it.
Discs
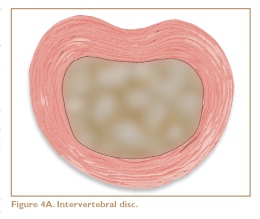
The phrase “slipped disc” is a popular misnomer. Spinal discs almost never slip, but they do crack and chip, and they may bulge and ooze out to place painful pressure on spinal nerves. Each disc is filled with a squishy substance and acts as a shock absorber, hydraulically cushioning the movement of the spinal bones. The lumbar discs are the thickest, probably because they absorb the most weight. They are roughly the diameter of a half dollar and are thicker in front than in back, conforming to the shape of the natural forward curve (Figure 4A).
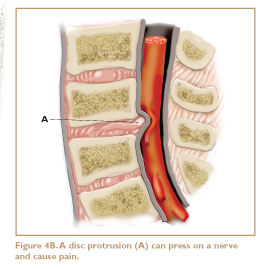
In a normal standing position, the lumbar discs are constantly pushed in an anterior direction. Therefore, if a disc is injured, it is more likely to protrude anteriorly, which causes little or no pain, than postero-laterally (to the back and side), where the nerves exit and a protrusion would cause more damage (Figure 4B).
Nerves
Discs and nerves are close neighbors. There’s not much room for the nerves in the low back (which control the hips, legs, and feet) to come through their openings in the spine, so any narrowing of their space can be problematic. The nerves that exit beneath the fourth and fifth lumbar vertebrae are the ones most frequently affected by disc problems. If the rim of a disc breaks and part of it presses against a nerve, this can cause numbness and weakness and/or pain in the back, hip, leg, and/or foot. Such injuries are relatively uncommon, however. Disc pressure on nerves accounts for only 2 percent to 5 percent of all back pain.
Low-Back Ligaments
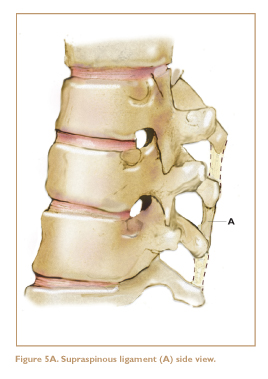
Other potential sources of aches and pains in the low back are strained ligaments. Several sets of ligaments help to hold the lower vertebrae together and keep the spine stable. The anterior longitudinal ligament and the posterior longitudinal ligament, located in front and in back of the vertebrae, respectively, embrace the discs and help to hold them in place. These are deep and are only occasionally injured. The three most commonly injured ligaments in the low back are the supraspinous, interspinous, and iliolumbar ligaments (Figures 5A, 5B, 5C).
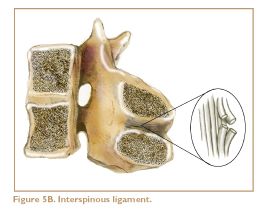
The supraspinous and interspinous ligaments connect the spinous processes, holding the back of the spine together. The iliolumbar ligament connects the fifth lumbar vertebra (L5) to the pelvis via the transverse processes of L5 and the ilium. When there are problems in this ligament, they usually occur at the portion of the ligament that attaches to the ilium.
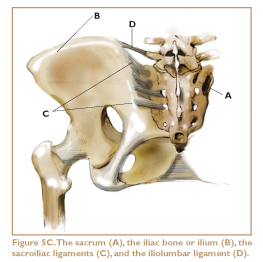
Sacroiliac Ligaments
In my experience, the main culprits causing low-back pain are not the structures in the low back proper, but those directly adjacent: the sacroiliac ligaments. The sacrum, a triangular bone at the base of the spine, is wedged in between the iliac bones; the sacroiliac ligaments attach those structures to one another. These massive, crisscrossing ligaments can be strained in many ways and in dozens of places. I will discuss sacroiliac ligament injuries in more detail in a future article.
Muscles
The erector spinae, quadratus lumborum, and iliopsoas are the major muscles that control movement in the low back and pelvis. The erector spinae group consists of hundreds of small muscles that run vertically from vertebra to vertebra, on either side of the spine. The quadratus lumborum attaches the posterior lip of the iliac crest to the twelfth rib and to the transverse processes of L1, L2, L3, and sometimes L4. The iliopsoas originates on the lateral anterior surfaces of the T12 to L4 vertebrae and the transverse processes of L1 to L5. It runs through the pelvis to the inside of the thigh and inserts at the lesser trochanter.
Any of these muscles may become strained, irritated, and painful, or they may pull the spine out of alignment and indirectly cause an ache in the low back. In addition, when a disc or ligament is damaged, these muscles frequently go into spasm (involuntary contraction). This contraction is a protective mechanism that serves to prevent movement that might increase the pain or cause further injury. Back pain purely due to muscle strain is usually of short duration. Muscles heal quickly — they are highly vascularized and are helped by many forms of treatment.
The Origins of Low-Back Pain—Direct and Indirect Causes
There are numerous “indirect” causes and very few “direct” causes of low-back pain. The indirect causes — emotional stress, poor diet, excess muscle tension, bone misalignment, a diminished craniosacral rhythm, inefficient movement habits, and others — frequently occur in combination and set the stage for the “last straw”: low-back injuries. Direct causes of low-back pain are the specific sources of actual physical damage: tears in muscle tissue, ligament sprains, sacroiliac joint inflammation, a disc pressing on a nerve root, etc.
Muscles in the low back are easily injured, but heal relatively quickly. Discs compressing nerves cause severe pain but account for only a small portion of injuries to the low back. Damage to ligaments, which leads to the formation of adhesive scar tissue, is the most common direct cause of chronic low-back pain. Ligament damage is also the least known and least understood of the various causes.
How It Happens
The following hypothetical scenario demonstrates the possible interrelationships between the indirect and direct causes of low-back pain. A person experiences significant emotional stress, which diminishes his craniosacral rhythm and leads to an increase in muscle tension. The tension increases the person’s anxiety, and he finds himself attracted to comfort foods high in sugar, fat, or caffeine. This produces additional stress in the body. The increase in abnormal muscle tension then pulls the bones slightly out of line, placing strain on the ligaments. The back pain that results is caused by swelling, mini tears, and adhesive scar tissue in the ligaments.
What convinced me that ligaments were the direct cause of most chronic low-back pain was the work of an unusually talented physician who had trained with Dr. James Cyriax. Over a period of several years, I observed patients with intractable back pain being test injected with xilocaine. For this procedure, the physician first identifies certain movements that recreate the pain the patient has been experiencing. This information helps to determine which ligaments may have been injured. Next, xilocaine is injected into these ligaments to see whether the pain temporarily disappears. If the person is then able to complete the formerly painful movements with little or no pain, the proper diagnosis has been established. Naturally, when the numbing medicine wears off, the pain will return; this is only a diagnostic procedure. The assessment is followed by targeted treatment aimed at healing the injured ligaments.
After seeing dozens of people who were assessed with test injections get well with subsequent treatment, I was convinced that ligaments play a critical role in back pain — and that hands-on therapy could provide lasting relief if the ligaments were treated directly with cross-fiber techniques. Of course, it is necessary to address the indirect causes of pain, as well as treat the ligaments; otherwise, the client’s improvement will only be temporary.
***
In the next article I will discuss in detail several of the most common ligament injuries affecting the low back, as well as effective assessment techniques for identifying these injuries.




