In the October/November 2003 issue of Massage & Bodywork (“Injuries of the Knee: Essential Principles and their Applications,” page 16), I described how discovering and learning new information about the injury process revolutionized my understanding and changed the way I treat clients in my practice. Because of the essential principles I learned, I am able to identify the source of clients’ pain quickly and recommend the type of treatment most likely to help them recover.
In the next three articles, I would like to focus on how the essential principles regarding pain, injury, and the body’s healing process can help us quickly assess and effectively treat our clients’ shoulder pain (often called “rotator cuff”) problems. The general term “rotator cuff injury” refers to one or more of four separate tendons in the shoulder. It is not a useful term unless the massage therapist can single out which of the rotator cuff tendons is injured. Most clients who come to you with a rotator cuff injury cannot tell you specifically what is wrong with their shoulder; in many cases, the physician who diagnosed the injury may not know exactly which tissues are injured, either.
The three specific shoulder injuries can be easily differentiated and treated: infraspinatus tendinitis, supraspinatus tendinitis, and subscapularis tendinitis. The fourth rotator cuff tendon is the teres minor and in my experience it is rarely injured. This article will focus on the first of these common injuries.
The Nature of Injury at the Infraspinatus Tendon
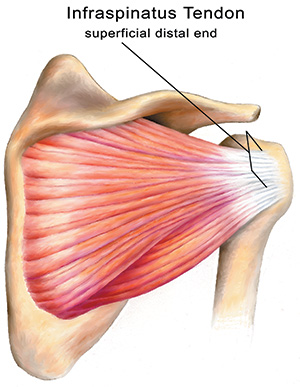
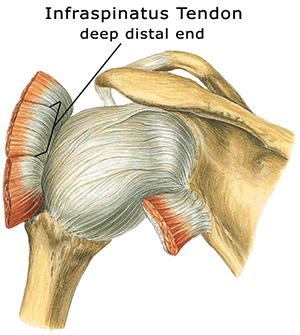
You use the infraspinatus muscle-tendon unit in a back-hand motion, when you write, open a door, or reach behind you. The muscle covers the lower portion of the scapula beneath the spine of the scapula, and its tendon attaches to the back of the greater tubercle of the humerus at the posterior upper arm. The infraspinatus muscle-tendon unit is responsible for lateral rotation of the shoulder. The infraspinatus tendon has a very large and broad tendon attachment, about a half-inch wide or more depending upon the size of the person. The body of the tendon is 1–2 inches long as well.
Because it has a poor mechanical advantage, the infraspinatus is a relatively weak muscle in most people. If it is called upon to suddenly perform heavy exertion, it can easily strain or tear. These lesions, or tissue damage, may be mild, moderate, or severe. Some people have a minor strain of the infraspinatus tendon that continues almost unnoticed for years. They may experience slight discomfort when reaching for something on a high shelf or into the back seat of the car. However, when this minor lesion does not heal properly, it can set the stage for a more severe injury later.
This tendon strain often occurs in people who play racquet sports and typically comes on slowly. This injury can occur when you hit a baseball, throw something into the back of your car, or pull off your shirt in an awkward manner. Infraspinatus tendinitis often persists for years, defying all attempts at diagnosis and treatment. The injury interferes with sleep, sports, and even everyday movements. It can be a very painful and tenacious injury.
Pain as a Signal of Infraspinatus Tendinitis
When a strain of the infraspinatus tendon occurs, the person frequently feels nothing at the moment because the tendon is warmed-up or because the person is focused in the heat of the moment during an athletic activity. Later that day or the next morning, he may have difficulty putting on a shirt or coat, as the arm is lifted up and out to the side. Infraspinatus tendinitis rarely causes pain in the infraspinatus muscle itself. In thinking about this injury, it is helpful to remember the concept of “referred pain”—when the client perceives pain in a part of the body at some distance from the injured tissues. One of the principles of referred pain is that the pain is felt distally, referred toward the periphery of the body from the true site of injury. With infraspinatus tendinitis, pain is felt in the upper-arm region, sometimes slightly toward the back of the arm, but not always. When the injury is severe, pain can be referred to the wrist.
Remember that referred pain is very convincing to the client. When testing for infraspinatus tendinitis, don’t pay too much attention to exactly where the client feels pain as long as it is felt in the arm or deltoid area. During the verification tests for this injury, pain will often be felt down the back, front, or outside of the upper arm and occasionally over the scapula. A client with severe infraspinatus tendinitis may complain of pain down the arm as far as the wrist, but this latter pain pattern occurs only in extreme cases of this injury.
Scar Tissue and Chronic Pain in Infraspinatus Tendinitis
The infraspinatus tendon is generally injured at one of two sites at the tenoperiostial junction (where the tendon attaches to the bone): (a) at the superficial distal end (the part of the tendon near the skin surface) or (b) at the deep distal end of the tendon (the part of the attachment deep near the bone). As mentioned, minor injuries at these sites may go almost unnoticed by the person until the buildup of adhesive scar tissue leads to chronic pain.
Injury Verification of Infraspinatus Tendinitis
The most important positive test for this injury is pain felt on resisted lateral rotation (see Test 1 on page 103). If the tendon is injured at the deep distal end of the tendon, then there will also be pain during another test: passive elevation of the arm (see Test 2). This test compresses the deep fibers of the tendon between the head of the humerus and the acromion. If the tendon is injured at the superficial distal end, then there is a so-called painful arc (see Test 3). This test compresses superficial fibers of the tendon between the head of the humerus and the acromion when the arm is approximately 70 degrees to 110 degrees from the body. If both of these auxiliary tests cause pain, then both the deep and superficial parts of the tendon are injured. If resisted lateral rotation (Test 1) is the only test that causes pain, then infraspinatus tendinitis is present in the body of the tendon. The latter is fairly uncommon.
Remember, the primary test for this injury is resisted lateral rotation. The secondary or auxiliary tests, Tests 2 and 3, give you auxiliary information so you know where in the tendon structure the injury is located. Test 2 is passively done by the therapist. Test 3 is actively done by the client. This information is important in understanding how hard to press if you are applying cross-fiber friction therapy.
Test 1: Resisted Lateral Rotation

Image 1A: Resisted lateral rotation test
Have the client stand with her legs at least shoulder-width apart so she is stable while doing the test. Place one hand on her upper arm just above the elbow and press the upper arm into the body for stability. With the person’s arm bent in front at a right angle, place your other hand on the outside of her lower arm just above the wrist. Now ask the client to push laterally or outward toward you while you resist the push with equal force (Image 1A). This test is done at 90 degrees to the body, first, but also may need to be done at 30 degrees (Image 1B) and at 135 degrees (Image 1C) for more precise testing. The different angles put stress on different parts of the tendon. A positive test, when pain is felt, indicates that the infraspinatus is injured.

Image 1B: Rotate client's arm inward to 30 degrees and repeat test for more precise results

Image 1C: Rotate client's arm outward to 135 degrees and repeat test for more precise results
Test 2: Passive Elevation
First, say to the client, “Raise your arm above your head.” This test is to see if the person can actually raise her arm. Then place one hand on the elbow and your other hand at the back of the same shoulder to stabilize the joint. Now push the arm back behind the client’s head diagonally until you come to the very end of the range of movement (Image 2). If there is still no pain, give the arm a slight jerk in the same direction. This jerk is always done at the very end of the range of motion, and the person is totally relaxed while you passively test the arm. Pain on this test indicates that the deep distal end is injured.

Image 2: Passive elevation test
Test 3: The Painful Arc Test
Ask the client to lift the arm slowly out to the side until the arm is raised above the head. Instruct the client to stop if there is any pain and then to continue the motion to see if the pain ceases. Pain on this test between 70 degrees and 110 degrees indicates that the superficial distal end of the infraspinatus tendon is injured.
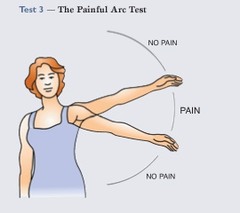
Image 3: Painful arc test
Healing Injured Tissues in Infraspinatus Tendinitis
Two to three months of rest will sometimes allow infraspinatus tendinitis to heal, but more often it will remain for years, especially in an active person. The tendon injury exercise program, along with rest, may improve the condition. Treatment is usually recommended if rest and exercise don’t eliminate the pain in the course of a month. Hitting backhand in racquet sports is not a good idea while the client is in treatment, nor are any exercises that cause pain. Push-ups and chin-ups are two of the worst offenders when this injury is present. Here is a description of four treatment options.
Massage:
Massage alone is not usually an effective treatment for infraspinatus tendinitis. There is often very stubborn scar tissue that needs to be broken down as described below. Massage of the infraspinatus muscle is useful as an adjunct to friction and exercise therapy.
Friction Therapy:
If the tendon tear is not too widespread, then four to six weeks of friction treatment are usually effective. Friction therapy reduces adhesive tissue and helps the tendon to heal correctly. The therapy should not be painful, just a little annoying.
Location and Friction of the Infraspinatus Tendon
The client is lying on her side on the table with the injured side up. The injured arm hangs off the table at shoulder level. Run your finger outward along the spine of the scapula (the bony ridge that separates the upper and lower scapula). As you reach the lateral end of the spine of the scapula, drop down about a half inch to the medial aspect of the greater tubercle of the humerus; this is the most common site of injury. Move horizontally across the arm to apply transverse friction with the thumb or forefinger for 10–12 minutes (Image 4). Take a break after five or six minutes to give both of you a rest.

Image 4: Applying transverse friction to the infraspinatus tendon
Exercise Therapy:
This tendon exercise program is very effective if done daily for six to eight weeks.1 The stretching realigns the scar tissue fibers so they can heal correctly, and the weight-calibrated exercises systematically increase the strength of the tendon. If the client’s personality is such that she will not do it consistently, this is not the program to recommend. In these cases, try only giving the client strengthening exercises. There are five steps to the program: warm-up, stretch, exercise, stretch, and ice or heat.
1. First, have the client warm up the tendon by circling the arm for two or three minutes. Ask her to stand with the arm 3 or 4 inches in front of the body and make a wide, slow circle.
2. Stretch the tendon five times for 30 seconds each time. This stretch mimics passive adduction. The person crosses the arm in front of the body, bringing the elbow of the affected arm toward the opposite shoulder. Have her place the other hand on the elbow, then pull in toward the opposite shoulder (Image 5). Make sure the elbow is on the same or a slightly higher level with the shoulder, not below it. Only a slight pull, not pain, should be felt in the shoulder. Rest a moment between stretches, and be sure to hold each stretch for the full 30 seconds. Repeat five times.

Image 5: This stretch mimics passive adduction
3. This exercise mimics resisted lateral rotation. Have the client lie on a bed on her side with the injured side up. Allow the hand of the injured arm to hang down, keeping the elbow and upper arm against the body (Image 6).

Image 6: This exercise mimics resisted lateral rotation
Hold a 1- to 5-pound weight and lift the hand, rotating toward the ceiling until the arm is at a 180-degree angle to the body (Image 7). Do three sets of 10, feeling stress in the last 10 only.

Image 7: Holding a weight in her hand, the client rotates her arm toward the ceiling until a 180-angle degree is reached
For this exercise program to be effective, only the third set of 10 should cause some tiredness or distress. This challenges the tendon structure and causes it to strengthen. If there is no sense of tiredness, not enough weight is being used. Try again the next day with a little more weight—begin with 1 to 3 pounds. If fatigue or distress is felt during the first 10 or 20 repetitions, too much weight is being used. Stop and begin the next day with less weight. If there is pain with little or no weight, wait a week and try again.
On the first day of the second week, increase the amount of weight to that which will cause slight tiredness (usually 1 pound) in the last 10 repetitions. Of course, if it is still causing some fatigue for the client, keep her at this level of weight a little longer. At the beginning of each new week, increase the weight again. Do this each week for six to eight weeks.
4. Stretch five times for 30 seconds each, exactly as in Exercise 2.
5. Apply ice or heat to the affected area for 5–10 minutes.
This program must be done every day, seven days a week to be effective. It is usually done once a day at first, but should be done twice a day after about two weeks. Afterward the client may feel slight discomfort for several hours. This distress is fine unless soreness lasts for several days. If the discomfort persists, discontinue the program and try again a week later.
Injection:
One or two corticosteroid injections given by a physician trained in orthopedic medicine are usually effective (a physician trained in non-surgical treatment of musculoskeletal pain). This injection should be followed by several days of rest and six weeks of rehabilitation. One or two injections of proliferant are effective in chronic cases where the tendon has been distended and weakened. The proliferant stimulates the build-up of strength in the tendon. The rehabilitation exercises outlined above should be used during this period.
Principles at Work
Usually one of these treatment modalities works. The longer the person has had infraspinatus tendinitis, the longer and more difficult the treatment will be. Use your intuition and your instincts with these skills once you are comfortable with them. The more cooperative the client is in maintaining the exercise routine, the shorter the duration of treatment. Remember, once the client begins to get better, the danger of reinjury increases because the injury isn’t fully healed, even though the person feels better. Encourage your client to return to full activity very slowly or she will likely get reinjured.
Note
1. Curwin and Stanish, “Tendinitis: Its etiology and treatment,” (D.C. Heath and Company, 1984).




