By Ben E. Benjamin, PhD

If you’ve strained one of your fibularis tendons, the pain in your ankle will let you know something is wrong, but you’ll probably have a hard time identifying the fibularis as a source of the trouble. That’s because this injury tends to get overshadowed by a much more common and better-known cause of pain: a lateral ankle sprain.
In fact, the fibularis usually doesn’t get injured in isolation. Typically the ankle is sprained as well. But when a fibularis muscle or tendon is involved, simply treating the sprained ligaments will not fully resolve the pain.
There are three fibularis muscles: the fibularis longus, brevis, and tertius (Image 1). The fibularis tertius is a very small, weak muscle that is not usually injured. The two stronger muscles begin at the lateral lower leg, just inferior to the knee, and travel down toward the ankle. Their tendons begin just superior to the ankle and wrap around the back of the lateral malleolus in a little groove, where they are held in place by a band-like structure called the superior fibular retinaculum (formerly the superior peroneal retinaculum). These two tendons are wrapped in a sheath until they part company, with the longus tendon running through the foot and attaching to the first metatarsal bone and the brevis attaching to the fifth metatarsal bone. The major function of the fibularis muscle-tendon units is to stabilize your lower legs as you walk so that your ankles don’t wobble and give way laterally. The longus (“the long one”) helps you to move your foot in eversion when the foot is plantar flexed, while the brevis (“the short one”) lets you evert the foot when it’s in a dorsiflexed position. Of course, whenever you move into eversion, both of these muscles are active, but depending on the foot position, one will be more dominant.
Image 1:
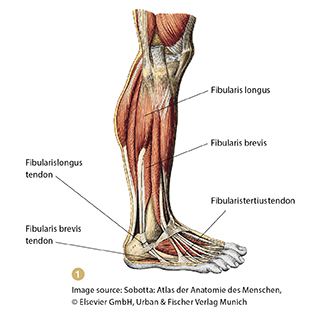
The fibularis longus and brevis act as a counterbalance to the posterior tibialis muscle, which I discussed in a previous article (“Posterior Tibialis Injuries,” September/October 2009, page 102). Together, they are referred to as the stirrup muscles. Imagine sitting on a horse and pressing down on just one stirrup—you would be unstable and more likely to fall off. Likewise, if your fibularis and posterior tibialis muscles are not in balance, you are much more likely to fall and sprain your ankle. These structures are placed under stress whenever you walk on uneven ground, climb on rocks, go skiing, or run quickly from side to side as you might in a tennis or basketball game.
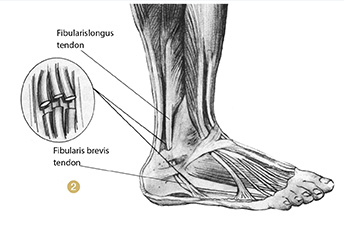
Injuries to the fibularis tendons may cause pain at the lateral aspect of the lower leg just above or below the lateral malleolus or at the outside of the foot below the ankle (Image 2). If the muscle belly is injured, pain is felt between the lateral knee and the lateral ankle. The most common site of injury is directly posterior to the lateral malleolus.
Image 2:
How and Why These Injuries Occur
Fibularis muscle and tendon injuries may occur suddenly as a person walks on very uneven ground, steps into a hole while walking or running, slides into second base, or gets tripped in a soccer match, or in any other accident in which the ankle turns with the foot beneath the body. More frequently, though, the injury develops slowly over time as a result of overuse or a chronic misalignment of the foot. Our feet are extremely complex structures—containing 26 bones, 20 different muscles, and more than 50 ligaments—and they need to support the entire weight of our bodies. There are many opportunities for things to go wrong.
For instance, if some of the bones in the feet are out of alignment or if the medial arches are congenitally high, the feet may naturally begin to pronate, causing the arches to fall. When this happens to people, they feel like they are walking with their knees turned inward, as though they are pigeon-toed. They will tend to compensate by turning their feet out 10, 20, or 30 degrees and walking in this misaligned position where the feet are angled out and the knees are pointing straight ahead. That creates a torque in the knees, ankles, and hips, causing stress to ricochet throughout the body, all the way up to the neck.
In this position, the weight going through the feet and legs shifts medially so that more of the body’s weight falls onto the metatarsal of the great toe, the medial ligaments of the knee, and the muscles of the medial leg—particularly the medial aspects of the soleus and gastrocnemius and the posterior tibialis muscles. Much less weight is supported by the fibularis longus and brevis. As a result, all of these muscles and tendons become more vulnerable to injury. While the medial structures fatigue from overuse, the lateral structures begin to weaken and atrophy. When a weakened fibularis muscle-tendon unit is then suddenly called upon to do its job, it can easily tear under the strain.
Fibularis injuries occur frequently in athletes, dancers, and runners. Typically the first sign is an ache in the lateral lower leg or just behind the lateral malleolus. Over time, the person feels increasing pain and may begin to limp if the injury becomes severe. As mentioned earlier, pain in the ankle region is frequently confused with (and frequently coexists with) a lateral ankle sprain.
Injury Verification
When one of the fibularis tendons is strained, it often hurts just to walk or rise up on the ball of the foot. Usually the greatest pain is felt when everting the foot against resistance.
Test 1. Resisted Eversion In Dorsiflexion (Tests The Fibularis Brevis)
Sitting at the base of the table facing the client’s foot, place your medial hand under the heel for support and your lateral hand on the lateral aspect of the foot. Then, ask the client to forcefully push outward (laterally), keeping the foot in a dorsiflexed position as you push medially with equal and opposite force. If the fibularis brevis is injured, the client will feel pain at the lateral ankle or in the lateral lower leg (Image 3).
Image 3:

Test 2. Resisted Eversion In Plantar Flexion (Tests The Fibularis Longus)
Perform the same action as in the previous test, but with the foot in plantar flexion. This position stresses the fibularis longus more than the brevis. If the structure is injured, the client will feel pain at the lateral foot or ankle or in the lower leg (Image 4).
Image 4:

Palpation Testing
The fibularis brevis and longus tendons are easy to access, particularly if the client everts the foot. Palpate just posterior and superior to the lateral malleolus. An injured tendon will be sore on palpation.
Treatment Choices
Self-Treatment
As with many different soft-tissue injuries, it’s important for the client to stop strenuous activity immediately. If the injury is not severe, the rehabilitation exercises described below may be sufficient to help the person recover fully. For very minor strains, rest alone sometimes does the trick. If the pain lasts more than a week or so, treatment is recommended.
Friction Therapy
Friction therapy is a form of dry, cross-fiber massage that creates a mild, controlled trauma in an injured tissue. It facilitates healing in several ways:
•Breaking down scar tissue.
•Separating ligament-to-bone adhesions.
•Increasing circulation.
•Promoting the formation of properly aligned and mobile tissue.
•Promoting collagen formation, in cases of tendinosis.
I have found friction therapy to be extremely effective in treating fibularis muscle and tendon injuries.
Treating the tendons.
Sit facing the client’s foot, holding it in inversion and adduction so that you stretch the lateral tendons, and palpate the tendons to find the injured area or areas. These will usually be located above or slightly behind the lateral ankle. Place two or three fingers on the injured fibers, and place your thumb on the medial side of the lower leg to stabilize your hand (Image 5). Now move your wrist and arm, applying friction pressure up against the fibula in one direction only.
Image 5:

Treating the muscles.
With the client lying supine, use palpation to identify the painful area(s) of the muscle and apply friction at a 90-degree angle to that muscle tissue. Generally, it is easiest to brace on the medial lower leg with your fingers and perform the friction with your thumb. Use whatever position is most comfortable for you; there is no right position.
Massage Therapy
After frictioning the injured areas, perform transverse massage and effleurage to the entire leg to maximize circulation.
Exercise Therapy
Outer-Ankle Lift
This exercise requires the use of props—either weights that attach to the foot in some way or a small plastic shopping bag containing a one- to five-pound weight. It is performed from a side-lying position on a couch or bed. Have the client start with the knees bent, injured ankle on top, and then extend the top leg off the edge of the couch or bed (while wearing the weight or the shopping bag). Then, have the person lift the outside of the foot toward the ceiling—10 times with the foot in plantar flexion and then another 10 with the foot in dorsiflexion (Images 6 and 7). Build up slowly to three sets of 10 repetitions in both foot positions.
Image 6: Image 7:


Inner-Ankle Lift
This exercise requires the same props as the Outer-Ankle Lift, but is done from a sitting position. To begin, have the client sit in a chair and cross the injured leg over the good leg, with either the weight apparatus or the loaded shopping bag across the forefoot (the front part of the foot, just behind the toes). Now instruct the client to raise the foot toward the ceiling 5–10 times, take a brief rest, and repeat (Images 8 and 9). Don’t use too much weight to start; begin with a lighter weight and gradually build up to using 5–10 pounds over the course of the treatment. The client should begin to feel tired after 5–10 repetitions.
These exercises should not cause any pain. If either of them does, it means the person is using too much weight or is not yet ready to begin that exercise.
Image 8: Image 9:

Active Isolated Stretching Technique
Practitioners who are trained in Active Isolated Stretching (AIS, described in my articles in the May/June 2010 and July/August 2010 issues, pages 88 and 90, respectively) will want to perform a number of AIS techniques for the lower leg. The following stretch targets the fibularis muscles and is particularly beneficial.
To stretch the fibularis, lift the leg on the injured side until the hamstring is taught and the knee wants to bend. Now put the lower calf on your shoulder and ask the client to invert the foot. Wrap your hands around the foot and ask the person to pull the toes toward the nose (dorsiflex the foot). Do this about 10 times, stretching for no more than two seconds each time.
Orthotics
In some cases, an orthotic device can help to relieve stress on the muscles and tendons of the foot, helping to prevent future damage from occurring. If you think that foot alignment or structural issues may have contributed to the client’s injury, refer the person to a podiatrist.
Conclusion
The fibularis brevis and longus play an important role in supporting the lateral foot, leg, and ankle. When these structures get injured, the most important step is an accurate assessment, which can sometimes be tricky; in particular, it’s easy to overlook a fibularis tendon injury when a lateral ankle sprain is present as well (which happens quite frequently). Once you’ve pinpointed the damaged fibers, the treatment for these easily accessible structures is relatively straightforward. When treatment is given twice a week, standard healing times are 4–6 weeks for minor strains and 8–12 weeks for more serious strains, with many clients healing more quickly. Overall, the long-term prognosis for these injuries is very good.




